AIEM Clinical Podcast: Spinal Motion Restriction
AIEM
28-year-old PVA patient complaining of neck pain…
The typical trauma patient. South Africa has a huge trauma population that only seems to be getting larger! Spinal motion restriction is used every day, often with patients who don’t need it, or applied in a way that may result in more harm than good.
This post and podcast covers a broad spectrum of information for the application of Spinal Motion Restriction specific to the South African Environment.
This post and podcast covers a broad spectrum of information for the application of Spinal Motion Restriction specific to the South African Environment.
LSS: for the Long Story Short summary scroll to the bottom
SMR – What is it?
Spinal motion restriction refers to restricting a patient spine to prevent injuries from getting worse. We can use a bunch of different devices and methods to “hold c-spine”. Which ones are good, and which should we get rid of?
What devices can be used?
There are a variety of ways that we can ensure that spinal motion restriction can be applied. Starting from the most basic, we have self-immobilization. Asking an awake patient to hold their own head and neck still is a great way to keep a patient’s spine still.
If a patient has true pain on their C-spine, they will instinctively hold their own neck still 2.
If a patient has true pain on their C-spine, they will instinctively hold their own neck still 2.
Hard/soft collars have fallen out of favor and for good reason. There is currently no evidence that they are beneficial to patients, and there is a some evidence showing that they cause more harm than good1.
For some reason, they are still used and can be found on most ambulances. We discuss the possible use of these devices only for the movement/extrication of a patient out of a space, if they are unable to maintain their own C-spine due to level of consciousness.
Spine (trauma) boards. These boards were designed as an extrication device only, to assist with the removal of patients from vehicles and in rescue situations. They are NOT immobilization devices.
There is lots of evidence that has shown that prolonged periods on a spine board can cause respiratory compromise, pressure wounds, pain, and claustrophobia2.
Standing takedowns are worthless – we’re not going to waste our time with this. More information can be found in the ITLS Position Statement on the use of these devices.
There is lots of evidence that has shown that prolonged periods on a spine board can cause respiratory compromise, pressure wounds, pain, and claustrophobia2.
Standing takedowns are worthless – we’re not going to waste our time with this. More information can be found in the ITLS Position Statement on the use of these devices.
Scoop stretchers are a level up from spine boards, as they are rounded to allow for more comfort. Ideally, patients should still not be kept on one for a long time, as it can still cause pressure wounds. Scoop stretchers are also poor insulators, and a risk of hypothermia is present2.
So what is the gold standard for spinal motion restriction? We want a device that doesn’t cause pain, prevents pressure wounds and is comfortable for the patient.
Vacuum mattresses are currently the best device used to apply spinal motion restriction from a comfort and patient safety point of view. Be careful to ensure that temperature management is a concern as long periods of time in hot environments can result in patients overheating easily.
In hospital, you have better options in terms of patient comfort. Lying a patient supine on a hospital bed with head-blocks can be an effective way to keep SMR.
When do we apply SMR?
“Not all trauma patients are created equal “– South African Proverb
We see a lot of trauma patients in SA. It becomes difficult to identify a true spinal injury, but a proper assessment and the use of validated tools can help us recognize the injury.
Things to look out for:
- pain over the spine on palpation or movement
- obvious deformity of the spinal column
- unexplained hypotension coupled with absence of a tachycardia
- decreased motor and sensory function in upper or lower extremities - including pins-and-needles or loss of sensation (numbness)
- weakness or loss of movement (paralysis).
In penetrating trauma, SMR is not indicated unless the patient has the above signs and symptoms, and if the benefit of SMR outweighs the risk (mortality increases for the patient with penetrating trauma when we spend time with SMR rather than getting them to a theatre for definitive management).
How do we clear C-spine?
There are a handful of different guidelines that we can use to ‘clear’ C-spine, and they can help guide us in determining which patient should have SMR applied. It is out of the scope of practice of a Basic Ambulance Assistant (BAA) to ‘clear’ the c-spine.
The Canadian C-Spine Rule is the one most used and widely advocated for. As per the 2018 Clinical Practice Guidelines, all prehospital providers can apply spinal motion restriction – “[Including] the use of all evidence-based spinal motion restriction devices”.
The Canadian C-Spine Rule is the one most used and widely advocated for. As per the 2018 Clinical Practice Guidelines, all prehospital providers can apply spinal motion restriction – “[Including] the use of all evidence-based spinal motion restriction devices”.
Canadian C-Spine Rule
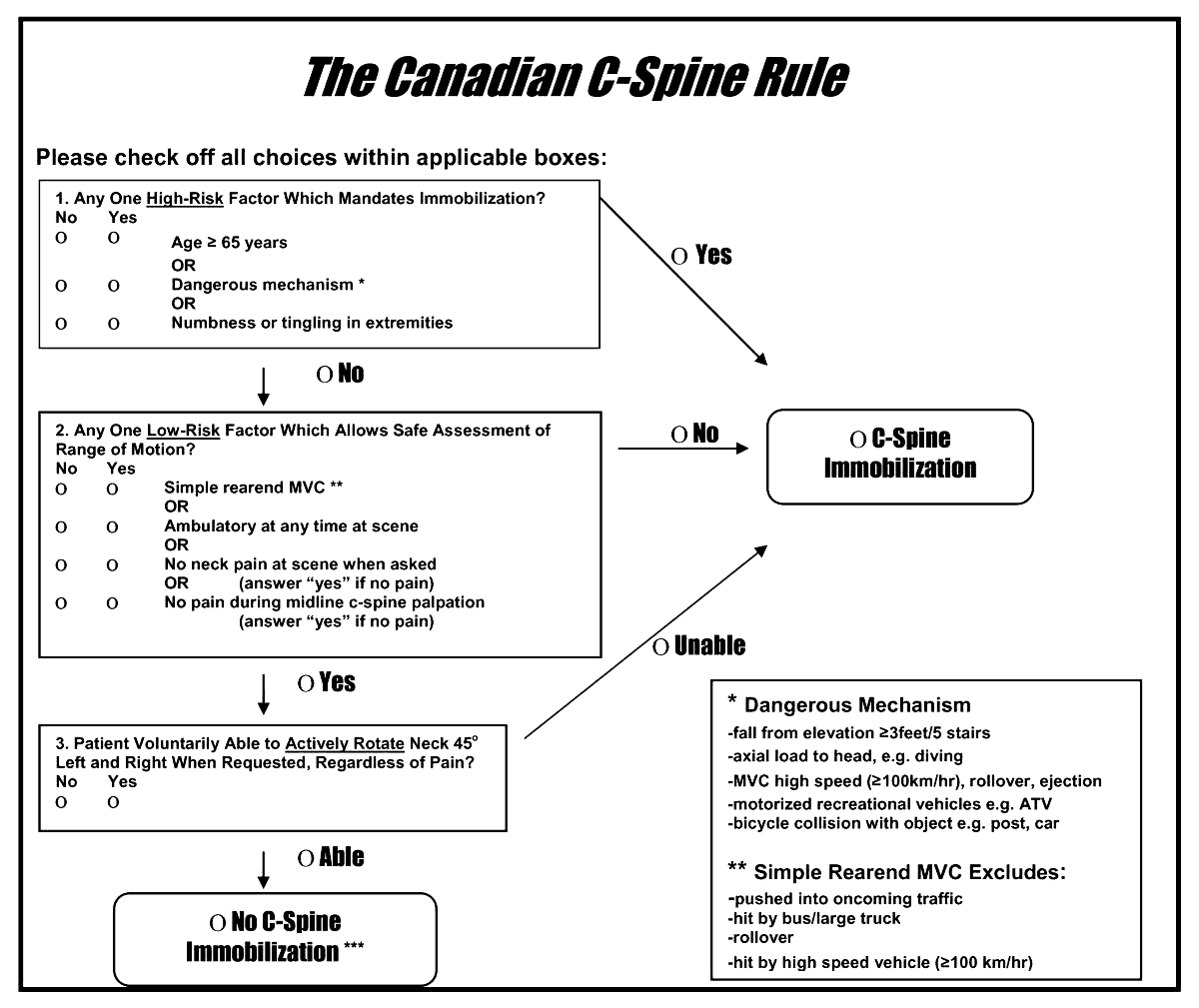
(this has been validated for pre-hospital and in-hospital use)
Long story short:
- Spine/Trauma boards are out! (except to extricate)
- Vacuum Mattress are in!
- Standing takedowns are only fun for the provider and don’t provide any benefit
- Hard collars are probably not ideal for most situations
- Follow a rule to determine risk and therefore apply SMR or not
- Assess your patient thoroughly and DOCUMENT your findings throughout the patient interaction
References
1 – Sundstrøm T, Asbjørnsen H, Habiba S, Sunde GA, Wester K. Prehospital use of cervical collars in trauma patients: a critical review. J Neurotrauma. 2014;31(6):531-540. doi:10.1089/neu.2013.3094
2 – Stanton D et al. Cervical collars and immobilisation: A South African best practice recommendation. Afr J Emerg Med, (2017), doi.org/10.1016/j.afjem.2017.01.007. https://www.thennt.com/nnt/cervical-spine-motion-restriction-blunt-trauma/
2 – Stanton D et al. Cervical collars and immobilisation: A South African best practice recommendation. Afr J Emerg Med, (2017), doi.org/10.1016/j.afjem.2017.01.007. https://www.thennt.com/nnt/cervical-spine-motion-restriction-blunt-trauma/
Subscribe to our newsletter!
Keep up to date with medical news, announcements about our courses and so much more.
Thank you!

-
23 Hobart road, Bryanston
Sandton, 2191
Quick Links
Copyright © Africa Institute of Emergency Medicine 2024

-
23 Hobart road, Bryanston
Sandton, 2191 -
Training@aiem.co.za
-
0861 374 7687
Quick Links
Connect with us
Copyright © Africa Institute of Emergency Medicine 2024
Special Date Request
Cant find the right booking date for you?
Leave us your details and we will try our best to fit you in.
Leave us your details and we will try our best to fit you in.
POPUP TEMPLATE FOR ALL COURSES
Johannesburg
Mpumalanga, Free State, North West, Limpopo, Northern Cape
Western Cape, KwaZulu-Natal, Eastern Cape
Request a date
Cant find the right booking date for you?
Leave us your details and we will try our best to fit you in.
OHS for Managers - Legal Liability Knowledge of OHSA
Johannesburg
Mpumalanga, Free State, North West, Limpopo, Northern Cape
Western Cape, KwaZulu-Natal, Eastern Cape
Request a date
Cant find the right booking date for you?
Leave us your details and we will try our best to fit you in.