Disjointed – a quick update on shoulder dislocations
AIEM
Glenohumeral joint dislocations are the most commonly dislocated major joint in the body.
Predisposed by a lack of intrinsic bony stability (the joint is very shallow) together with a wide range of motion. Anterior dislocations by far the most common type. Mechanism might help predict the type of dislocation – see below.
Find out about any numbness, tingling, weakness or history of prior dislocations. Identify associated injuries: BP, axillary nerve, radial nerve or axillary artery. Incidence of axillary nerve injuries increase with age (5 – 54%).
Predisposed by a lack of intrinsic bony stability (the joint is very shallow) together with a wide range of motion. Anterior dislocations by far the most common type. Mechanism might help predict the type of dislocation – see below.
Find out about any numbness, tingling, weakness or history of prior dislocations. Identify associated injuries: BP, axillary nerve, radial nerve or axillary artery. Incidence of axillary nerve injuries increase with age (5 – 54%).
Management
Recommendations
Treatment algorithm
Procedural sedation and full relaxation ensure a smooth and simple reduction. See ERC protocols:
Medication options include, but are not limited to:
- Early restoration on the anatomic position of humeral head – with time reduction success decreases due to local swelling.
- Recognition of other injuries associated with dislocations or reduction.
- Immobilization to prevent recurrent dislocations.
Treatment algorithm
It is very painful and optimal analgesia is indicated as soon as possible. Options include, but are not limited to:
- Perfalgan: 15mg/kg (plus-minus an opioid)
- Fentanyl: 2 – 20mcg/kg
- Ketamine: 0.1 – 0.3mg/kg
- Morphine: 0.1mg/kg
- Penthrop: self-administered inhalation until desired effect is achieved
- Regional block if you are proficient with this skill.
Procedural sedation and full relaxation ensure a smooth and simple reduction. See ERC protocols:
- ‘Procedure Consent Form’‘
- Procedural Sedation Policy’
- Obtain written consent prior to procedural sedation and reduction.
- Preferably have one doctor for sedation and one doctor to perform the reduction.
Minimal mandatory monitoring:
- Blood pressure (frequently during sedation)
- Heart rate (ECG)
- Breath rateETCO2
- Pulse oximetry
Medication options include, but are not limited to:
- Ketamine: 1mg/kg over 2 -3 minutes
- Propofol: 0.5 – 1mg/kg over 1 – 5 minutes and titrated by 10 – 20 mg bolus injections as needed
Options for reduction of anterior dislocations
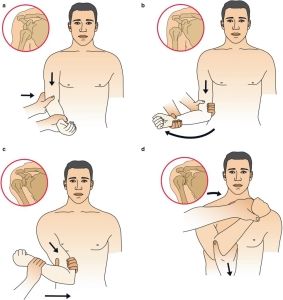
Kocher:
- Elbow flexed to 90 degrees and the arm then pressed (adducted) against the side of the body.
- After that slowly rotate forearm outward (75 degrees laterally) until resistance is felt, then the point of the elbow is lifted forwards and adducted.
- Finally the arm is rotated medially.
Hippocratic: simplest and most commonly method:
- Downward traction applied by clinician performing reduction.
- Assistant applies counter traction by holding a sheet wrapped around patient’s chest and under patient’s axilla and pulling it towards the patient’s contralateral shoulder.

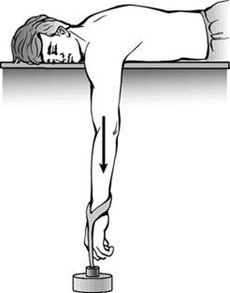
Stimson: helpful technique if is contra-indicated
- Patient prone, 3-5 kg weight at wrist.
- Apply gentle internal and external rotation. Reduction should occur within 20 minutes.
Milch
- With patient prone, place one hand on patient’s axilla and other hand holding patient’s hand.
- Gently abduct arm fully, then externally rotate and apply gentle traction for reduction
Write your awesome label here.
Scapular manipulation: quickest and safest option by repositioning glenoid fossa for reduction.
- With patient upright or prone with arm hanging off table, apply downward traction.
- Rotate inferior tip of scapula medially with direct pressure while rotating superior and medial edges lateral.
Reduction of inferior dislocations
Reduction of posterior dislocations
- Urgent orthopaedic consultation is necessary.
- Open reduction may be required.
- Closed reduction may be attempted under procedural sedation: traction applied in line with humeral shaft while an assistant applies counter traction. Gentle abduction usually reduces the dislocation.
- Associated brachial plexus- and axillary vessel injury is common.
Reduction of posterior dislocations
- Urgent orthopaedic consultation is indicated.
- Closed reduction may be attempted under procedural sedation: the arm is pulled and rotated laterally, while the head of the humerus is pushed forward.
Post-reduction management
- Urgent orthopaedic consultation is indicated.
- Closed reduction may be attempted under procedural sedation: the arm is pulled and rotated laterally, while the head of the humerus is pushed forward.
Advise to patient - Do a post-reduction X-ray to ensure that the reduction was effective.
- Ensure that the limb is neuro-vascularly intact post-reduction.
- Immobilisation with a sling: done with arm in internal rotation.
Duration of immobilisation depends on age of patient and complexity: - Generally 2-3 weeks in older patients
- Up to 6 weeks in younger patients with first dislocation
- Complex cases where there is associated fracture of humerus, rotator cuff tear, axillary nerve injury or recurrent dislocations should be referred to an orthopaedic surgeon early on.
Rehabilitation: - Refer to physiotherapist for early shoulder exercises prevent adhesive capsulitis.
- Discharge patients on adequate analgesia.
Dislocation – Pearls and critical points
- Document your serial neurovascular examinations.
- Evaluate for associated humeral head fractures.
- Unless urgent conditions contra-indicate pre-reduction films should be obtained in all patients.
- AP, lateral and Y views
- Post-reduction films are required on all reduced dislocations.
- AP, lateral and Y views
- Adequate analgesia and procedural sedation is crucial.
- Joint should be stabilized post reduction.
References
com [homepage on the Internet]. Johannesburg: Essential Medical Guidance 2020 [cited 2020 Sept 10]. Available from: https://emguidance.com/
Hodkinson P, Evans K, editors. Emergency Medicine Clinical Guidance for the Western Cape. 4th Cape Town: Divisions of Emergency Medicine; 2017
Solomon L, Warwick DJ, Nayagam S. Apley’s Concise System of Orthopaedics and Fractures. 3rd London: Hodder Arnold; 2005
Wallis LA, Reynolds TA. AFEM Handbook of Acute and Emergency Care. Cape Town: Oxford University Press Southern Africa (Pty) Ltd; 2015
Subscribe to our newsletter!
Keep up to date with medical news, announcements about our courses and so much more.
Thank you!

-
23 Hobart road, Bryanston
Sandton, 2191
Quick Links
Copyright © Africa Institute of Emergency Medicine 2024

-
23 Hobart road, Bryanston
Sandton, 2191 -
Training@aiem.co.za
-
0861 374 7687
Quick Links
Connect with us
Copyright © Africa Institute of Emergency Medicine 2024
Special Date Request
Cant find the right booking date for you?
Leave us your details and we will try our best to fit you in.
Leave us your details and we will try our best to fit you in.
POPUP TEMPLATE FOR ALL COURSES
Johannesburg
Mpumalanga, Free State, North West, Limpopo, Northern Cape
Western Cape, KwaZulu-Natal, Eastern Cape
Request a date
Cant find the right booking date for you?
Leave us your details and we will try our best to fit you in.
OHS for Managers - Legal Liability Knowledge of OHSA
Johannesburg
Mpumalanga, Free State, North West, Limpopo, Northern Cape
Western Cape, KwaZulu-Natal, Eastern Cape
Request a date
Cant find the right booking date for you?
Leave us your details and we will try our best to fit you in.