How to PPE Safely – COVID-19 Recommendations
AIEM
Personal Protective Equipment and their proper use will assist in protection against the COVID-19 and exposure to the virus for healthcare workers, ancillary staff and other people within the healthcare system.
Putting on PPE and getting it off again can present some serious challenges! First of all, what should I wear? Different hospitals and systems have different recommendations, however the NICD COVID-19 Disease: Infection Prevention and Control Guidelines provide the following guidance:
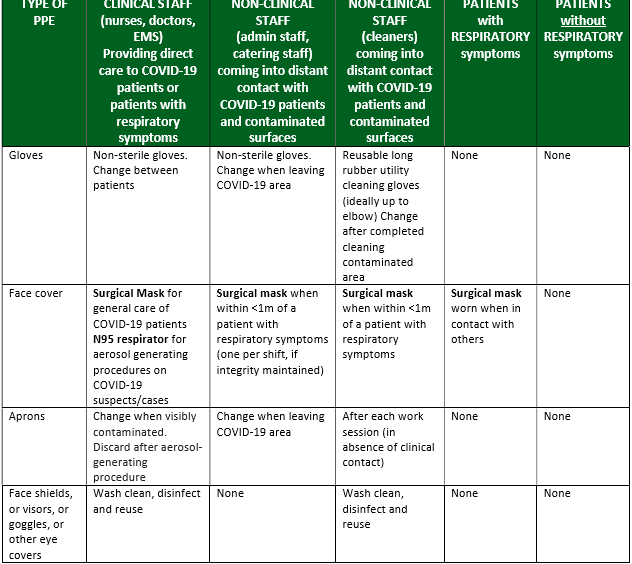
The PPE for clinical staff is different for those providing care with possible aerosol creation, and then those who are not at risk of aerosol creation. This changes the PPE requirement somewhat.
We will discuss the following:
- How to properly DON PPE for protection against aerosol creation
- How to DOFF PPE for these procedures
- What mask should I wear and when? (cloth vs surgical vs N95)
- What is the deal with gloves?
- Can I use PPE more than once?
Donning and Doffing PPE
The University of Cape Town has published some really useful videos on the application and removal of PPE before and after contact with patients where contact with possible aerosol of the virus may be a risk, watch the video linked below.
Write your awesome label here.
This process must be a slow and thoughtful process, being very careful not to expose yourself or others to any risk
1. Donning the PPE
- Clean hands using alcohol cleaner or washing your hands with soap and water
- Put apron (or gown) on (over your head and tie it at the back)
- Place the mask on your face (N95 if aerosol generating procedures will be performed)
- One strap above the ears and one strap below
- Mold the mask to the face and check a positive and negative pressure seal to make sure it fits the face really well
- Place goggles or face visor over the eyes, making sure they interface with the mask well and comfortably
- Make sure no hair gets trapped in the seal
- Apply gloves to your hands
Go and treat the patient as needed
2. Doffing procedure (this is the dangerous part)
You will need a bin (red bin to place all soiled items into)
Clean your hands after the gloves are removed (this will allow for any exposure with the gloves to be mitigated against)
Remove the apron
Remove the goggles
Remove the mask again, by avoiding contact with the front surface, using the elastic straps to pull the mask off your head and immediately place in a bin
Clean your hands and forearms immediately after the doffing procedure
If you are working in a COVID-19 ward and are moving from patient to patient, you won’t need to remove the goggles and mask with each interaction, only the gloves and gown. Remember to perform good hand hygiene between as noted above at each of the intervals noted above to avoid contamination of yourself or other patients. The re-use of PPE will be discussed later in this post, this will also depend on the system where you work.
Step 1 is to remove the gloves first. These will be the most heavily soiled pieces of equipment
- Peel the first one off and then place the clean finger under the cuff against your skin and peel off the second glove
- Place the gloves into the bin immediately
Clean your hands after the gloves are removed (this will allow for any exposure with the gloves to be mitigated against)
Remove the apron
- Using your hands to tear the apron from the back (where you tied it) or undo the knot you made to loosen the apron/gown
- Pull the apron/gown using the “clean” surface that was against your body, away from your body and allow the neck part to tear away from you (if you are wearing a gown this should be pulled forward to remove)
- Place the apron/gown in a bin immediately
Remove the goggles
- Avoid touching the front of the goggles and rather use your hands to pull the elastic of the mask off the head
- The goggles will need to be cleaned and disinfected according to your hospital’s policy
Remove the mask again, by avoiding contact with the front surface, using the elastic straps to pull the mask off your head and immediately place in a bin
Clean your hands and forearms immediately after the doffing procedure
If you are working in a COVID-19 ward and are moving from patient to patient, you won’t need to remove the goggles and mask with each interaction, only the gloves and gown. Remember to perform good hand hygiene between as noted above at each of the intervals noted above to avoid contamination of yourself or other patients. The re-use of PPE will be discussed later in this post, this will also depend on the system where you work.
3. What mask should I wear and when? (cloth vs surgical vs N95)
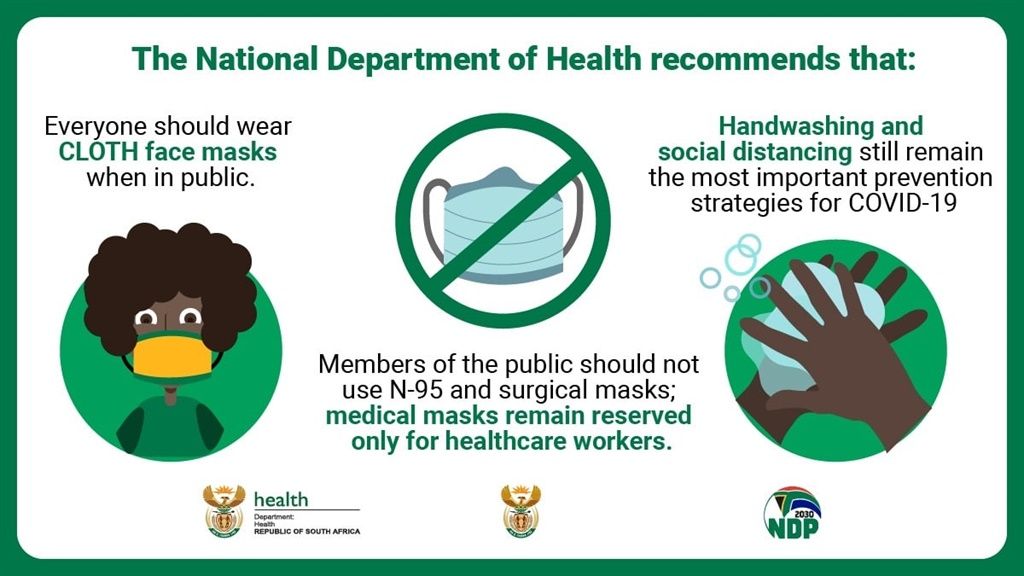
Cloth masks
These masks are not for use in the healthcare setting and are only recommended for use when people are out in public spaces. The mask does not provide the greatest protection. Social distancing and hand washing remain the best recommendation for prevention of spread.
Public areas of the hospital and areas where there is not likely to be exposure to a COVID-19 positive patient is where these masks might be used:
- Canteens
- Outdoor areas
- Public waiting spaces

Why not cloth masks for healthcare workers?
Cotton masks are not indicated for healthcare work because there is no filtration or protection against droplets or splashes. There is also the “wicking effect” which increases the risk of mucous membrane contamination. Cotton draws moisture towards the skin so if the cotton mask does get soiled, there is no protection for the healthcare worker. As this risk is low in a public space, the mask is recommended for use.
HOWEVER, if the mask does get soiled in a public space, it should rather be removed and replaced.
HOWEVER, if the mask does get soiled in a public space, it should rather be removed and replaced.
Cloth masks also need to conform to the following criteria to be helpful:
- The mouth and nose are fully covered
- The covering fits snugly against the sides of the face so there are no gaps
- There should be no difficulty breathing while wearing the cloth face covering
- The cloth face covering can be tied or otherwise secured to prevent slipping
- The cloth mask should be made of multiple layers of cloth
- The cloth mask must be washable and should be able to be ironable (these cloths should be washed after they are used each day)
Surgical Face Masks
These masks are for use in the healthcare setting for providers who are working in general wards and around patients who may present with possible COVID-19 infection. Any staff in contact with patients should ideally wear this kind of mask (reception staff, cleaning staff, clinical staff).
They are waterproof and provide protection against splashes and droplets. They are multiplayer masks and provide a higher level of protection.
Because these masks are specialized, they should be reserved for use by healthcare workers only.
They are waterproof and provide protection against splashes and droplets. They are multiplayer masks and provide a higher level of protection.
Because these masks are specialized, they should be reserved for use by healthcare workers only.


The following recommendations apply to these masks:
These masks are for use in the healthcare setting for providers who are working in general wards and around patients who may present with possible COVID-19 infection. Any staff in contact with any patient should ideally wear this kind of mask (reception staff, cleaning staff, clinical staff).
They are waterproof and provide protection against splashes and droplets. They are multilayer masks and provide a higher level of protection. Because these masks are specialized, they should be reserved for use by healthcare workers only.
They are waterproof and provide protection against splashes and droplets. They are multilayer masks and provide a higher level of protection. Because these masks are specialized, they should be reserved for use by healthcare workers only.
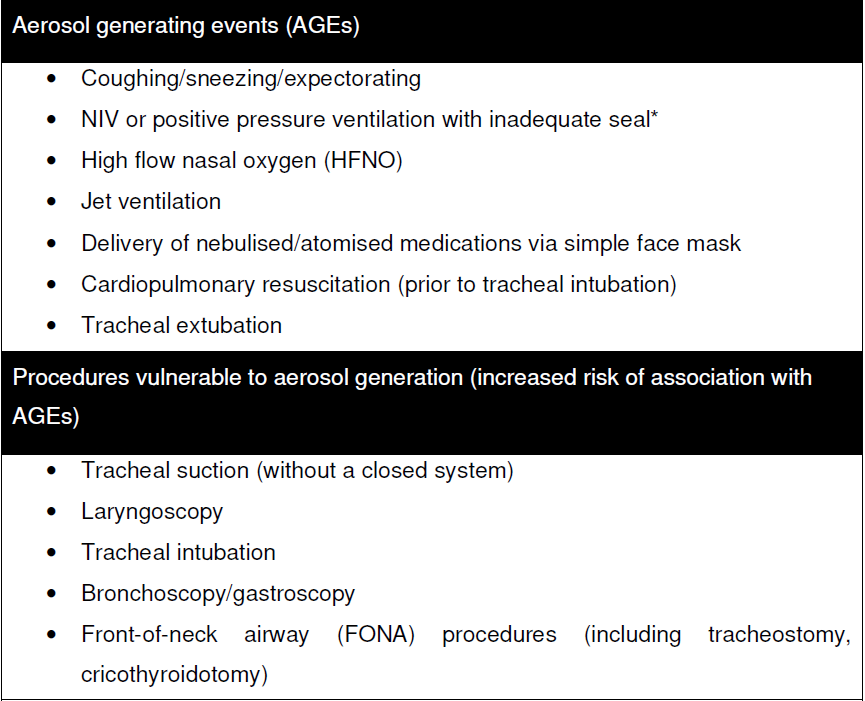
These masks are for use by healthcare providers only, and only when they are expecting to be exposed to a possible aerosol creating procedure.
These procedures can be found below:
Swabbing of the patient for COVID-19 testing is also considered high risk, and the appropriate PPE should be in place.
4. What is the deal with gloves?
Gloves are for use in single interaction situations where the hands need to be protected from possible exposure to the virus.
The general rule with gloves is to treat them as heavily soiled pieces of equipment, this means they should NEVER touch your face, your personal belongings, the inside of your pockets, your mask, or anything except the patient that is being treated at the time.
These are single use protective devices and should be used along with exceptional hand hygiene to manage the spread of infection.
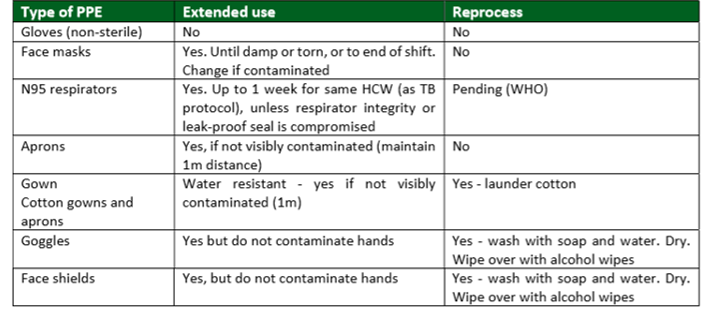
5. Can I use PPE more than once
The table below has been taken from the NICD SA guidelines which specify when and what PPE may be reused.
References
Department of Health. 2020. COVID-19 Disease: Infection Prevention and Control Guidelines Version 1 April 2020 . Published by the Department of Health. available online: https://www.idealhealthfacility.org.za/docs/Manuals-and-Handbooks/COVID%2019%20Disease%20Infection%20Prevention%20and%20Control%20Guidelines%20Version%201%20-%20%20April%202020.pdf [accessed: 08 May 2020)
Subscribe to our newsletter!
Keep up to date with medical news, announcements about our courses and so much more.
Thank you!

-
23 Hobart road, Bryanston
Sandton, 2191
Quick Links
Copyright © Africa Institute of Emergency Medicine 2024

-
23 Hobart road, Bryanston
Sandton, 2191 -
Training@aiem.co.za
-
0861 374 7687
Quick Links
Connect with us
Copyright © Africa Institute of Emergency Medicine 2024
Special Date Request
Cant find the right booking date for you?
Leave us your details and we will try our best to fit you in.
Leave us your details and we will try our best to fit you in.
POPUP TEMPLATE FOR ALL COURSES
Johannesburg
Mpumalanga, Free State, North West, Limpopo, Northern Cape
Western Cape, KwaZulu-Natal, Eastern Cape
Request a date
Cant find the right booking date for you?
Leave us your details and we will try our best to fit you in.
OHS for Managers - Legal Liability Knowledge of OHSA
Johannesburg
Mpumalanga, Free State, North West, Limpopo, Northern Cape
Western Cape, KwaZulu-Natal, Eastern Cape
Request a date
Cant find the right booking date for you?
Leave us your details and we will try our best to fit you in.